Blunt Chest Trauma and Chylothorax: A Systematic Review
Abstract
Introduction: Although traumatic chylothorax is predominantly associated with penetrating injuries, instances following blunt trauma, as a rare and challenging condition, are being increasingly documented. This study aims to systematically review the reported cases of blunt chest traumatic chylothorax (BCTC) and provide comprehensive insights into the condition.
Methods: Related studies published until December 11, 2024, were identified through Google Scholar. All studies documenting instances of BCTC, without restriction on cause or patient demographics, were included. Studies were excluded if they focused on chylothorax caused by penetrating injuries, their content was unretrievable, they were review articles, or they were published in blacklisted journals.
Results: Sixty-five eligible studies, encompassing 69 cases of BCTC, were included in the review. It predominantly affected males (73.91%), with patient ages ranging from 11 months to 84 years old. The most common clinical findings were dyspnea (47.83%) and abnormal auscultation or percussion (34.78%), with road traffic accidents as the primary cause (59.42%). Unilateral chylothorax was found in 72.46% of cases, bilateral chylothorax occurred in 27.54%, and pleural effusion was the most frequent radiological finding (55.07% in X-ray and 33.33% in computed tomography). Treatment typically included drainage (94.20%), parenteral nutrition (50.72%), and thoracic duct closure (39.13%). Most patients achieved complete recovery (89.85%), and six cases (8.70%) died.
Conclusion: The condition is rare and complex, underscored by the wide variability in patient demographics, clinical presentations, chylothorax onset, and management approaches. Given the challenges posed by limited evidence, the findings emphasize the need for early recognition and individualized management strategies.
Introduction
Chylothorax is a rare condition characterized by the accumulation of chyle in the pleural cavity caused by a disruption of the thoracic duct [1]. Chyle is an opalescent fluid that consists of triglycerides, chylomicrons, proteins, electrolytes, immunoglobulins, and fat-soluble vitamins, transported from the gastrointestinal system into the bloodstream by the thoracic duct. It makes up about 1-3% of total body weight in adults. Chylothorax was initially described by Bartolet in 1633 and later reported in the literature by Quinke in 1875 [1,2]. It is categorized into congenital, neoplastic, traumatic, and miscellaneous forms. The most common cause is malignancy, which leads to obstruction of the thoracic duct, while traumatic chylothorax is typically iatrogenic, resulting from surgical procedures or catheter placement. Penetrating trauma is the usual cause of traumatic chylothorax, while blunt trauma is considered an infrequent cause [1,2]. It may also develop due to chest compression or changes in intrathoracic pressure, such as during coughing or persistent vomiting [2].
The incidence of chylothorax is about 0.2% following blunt thoracic trauma and 0.9% after penetrating trauma. Bilateral chylothorax resulting from blunt trauma, mainly when no other injuries are evident, is an infrequent but severe complication [3]. Without prompt treatment, chylothorax can lead to serious complications, such as cardiopulmonary distress and significant nutritional deficiencies, with a high mortality rate of up to 15.5% [2-4]. Although traumatic chylothorax is predominantly associated with penetrating injuries, instances following blunt trauma have been increasingly documented, highlighting the need for awareness among healthcare providers regarding this potential complication [5,6]. This study aims to systematically review the reported cases of blunt chest traumatic chylothorax (BCTC) and provide comprehensive insights into the condition.
Methods
Literature search
The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Related studies published until December 11, 2024, were identified through Google Scholar using a search strategy that combined the following keywords with the “allintitle” and “including citation” features: (blunt trauma chylothorax), (blunt thoracic trauma chylothorax), (blunt thoracic injury chylothorax), (blunt chest injury chylothorax), (blunt torso trauma chylothorax), (blunt thoracic duct trauma), (blunt thoracic duct injury) and (traumatic chylothorax). The search was limited to English-language publications.
Eligibility criteria
All studies or reports documenting instances of BCTC, without restriction on cause or patient demographics, were eligible for inclusion. Studies were excluded if they focused on chylothorax caused by factors other than blunt chest trauma, if their content was unretrievable, if they were review articles, or if they were published in blacklisted journals. The legitimacy of the studies was verified by cross-referencing with widely recognized predatory journal checklists [7].
Study selection
First, an author conducted a literature search using the specified keywords and collected the relevant results. The titles and abstracts of the identified studies were then screened to exclude duplicates, non-English studies, and those unrelated to the study objective. Full-text screening was conducted for studies that passed the initial filtration, excluding those with unretrievable content or irrelevant study designs, such as reviews. This step was supervised by two authors, who independently reviewed each study. Finally, the remaining studies underwent legitimacy filtering.
Data extraction
The collected data encompassed various parameters, including the first author's name, year of publication, patient demographics, clinical manifestations, causes of chylothorax, chyle volume and content, the onset of chyle production, diagnostic methods, ICU admission status, treatment modalities, outcomes, and follow-up.
Statistical Analysis
The extracted data were organized in an Excel sheet (2019) and analyzed descriptively using the Statistical Package for the Social Sciences (SPSS, v. 27, IBM Co.). The results were presented in frequencies with percentages, means with standard deviation, and ranges.
Results
Study identification
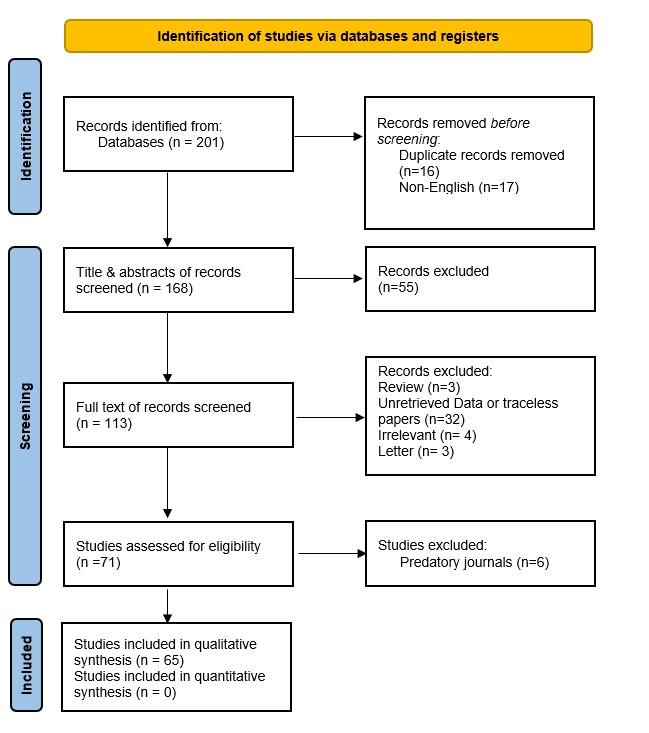
A systematic search yielded 201 studies, all of which were case reports. After removing duplicates (16) and non-English articles (17), 168 titles and abstracts were screened. Fifty-five case reports were excluded due to irrelevance, and full-text evaluation of the remaining 113 case reports led to the exclusion of an additional 42. Furthermore, six articles were excluded for being published in warning-listed journals. Consequently, 65 eligible case reports, encompassing 69 cases of BCTC, were included in the review [1-6,8-66] (Tables 1 and 2). The identification process is outlined in a PRISMA flowchart (Figure 1).
|
First author, year [Reference] |
Country |
Age (year) |
Gender |
CFP |
Cause |
SOC |
Amount of chyle (ml)/day* |
COAP (day) |
Biochemical content of chyle |
|
Harvey, 2024 [5] |
USA |
60 |
F |
Chest pain, multiple rib fractures |
RTA |
Left |
<500 |
2 |
Triglycerides |
|
Burduniuc, 2023 [2] |
Czech Republic |
70 |
F |
Blunt injury |
Fall on stairs |
Right |
>1000-2000 |
3 |
Protein, cholesterol, triglycerides |
|
Dung, 2023 [14] |
Vietnam |
32 |
M |
Thoracic spine injury, paraplegia |
RTA |
Right |
>1000-2000 |
At once |
Cholesterol, triglycerides |
|
Kim, 2023 [4] |
South Korea |
45 |
M |
Hemodynamically unstable, chest discomfort, multiple fractures, hemopneumothorax |
Crushed by a 2-ton metal frame |
Left |
>1000-2000 |
1.66 |
Triglycerides |
|
Boateng 2023 [33] |
USA |
75 |
F |
Respiratory distress |
Fall from bed |
Right |
<500 |
At once |
Triglycerides |
|
Ruest 2023 [34] |
USA |
15 months |
M |
Tenderness over right paraspinal thoracolumbar back, abnormal auscultation |
Child abuse |
Right |
N/A |
At once |
N/A |
|
Mohanakrishnan 2022 [35] |
USA |
70 |
F |
Dyspnea, back pain, abnormal auscultation |
Violent coughing episode |
Right |
>1000-2000 |
At once |
Chylomicrons, triglycerides |
|
Mazhar, 2021[23] |
UK |
42 |
F |
Dyspnea, abnormal auscultation |
Fall from horse 1 week before presentation |
Right |
>1000-2000 |
7 |
Triglycerides |
|
Waseem, 2021[32] |
Pakistan |
50 |
M |
Dyspnea |
RTA 2 days before presentation |
Bilateral |
>1000-2000 |
2 |
Triglycerides, cholesterol, fat-rich fluid with few inflammatory cells |
|
Din Dar 2021 [36] |
India |
50 |
M |
Blunt injury |
RTA |
Right |
>1000-2000 |
25 |
Triglyceride, chylomicrons |
|
Bacon, 2020 [9] |
USA |
53 |
M |
Hemopneumothorax |
RTA |
Left |
<500 |
5 |
N/A |
|
Champion, 2020 [12] |
Canada |
29 |
M |
Dyspnea, flushing, diaphoresis, vomiting, abnormal auscultation |
RTA |
Bilateral |
>1000-2000 |
At once |
Cholesterol, triglycerides |
|
Jindal 2019 [37] |
India |
35 |
M |
Dyspnea, respiratory distress |
RTA |
Bilateral |
>1000-2000 |
4 |
Triglyceride, WBC, albumin, glucose, protein, LDH |
|
Ahmed, 2018 [1] |
Iraq |
42 |
M |
Severe back pain |
RTA |
Right |
500-1000 |
2 |
Triglycerides and lymphocyte |
|
Brown, 2018 [10] |
USA |
53 |
M |
Thoracoabdominal injuries, subcutaneous emphysema, unstable pelvis |
RTA |
Left |
>1000-2000 |
N/A |
Triglycerides and lymphocyte |
|
Litzau, 2018 [22] |
USA |
66 |
F |
Dyspnea, multiple fractures, abnormal auscultation |
RTA 7 days before presentation |
Right |
>1000-2000 |
7 |
Triglycerides |
|
Kozul, 2017 [19] |
Australia |
18 |
M |
Multiple injuries |
RTA |
Bilateral |
500-1000 |
0.46 |
N/A |
|
Lee, 2017 [21] |
South Korea |
70 |
M |
Hemothorax, flail chest |
RTA |
Right |
>2000 |
5 |
Triglycerides, cholesterol |
|
Mohamed, 2017 [3] |
USA |
51 |
M |
Dyspnea, chest pain, abnormal auscultation |
Fall on stairs |
Bilateral |
>1000-2000 |
5 |
Triglycerides, Leukocytes, RBCs, LDH, protein |
|
Spasić, 2017 [6] |
Serbia |
55 |
F |
Multiple injuries |
RTA |
Right |
>2000 |
5 |
N/A |
|
Sriprasit, 2017 [31] |
Thailand |
27 |
F |
Hemothorax, neurogenic shock, multiple fractures |
RTA |
Left |
<500 |
5 |
Triglycerides, protein, glucose, LDH |
|
Hara 2017 [38] |
Japan |
17 |
F |
Breathing difficulty, abnormal percussion |
Recurrent chylothorax, physical punishment |
Left |
500-1000 |
At once |
N/A |
|
Jahn 2017 [39] |
Germany |
8 |
F |
Respiratory distress, abnormal percussion, and auscultation |
Pedestrian hit by a motor vehicle |
Left |
<500 |
5 |
Protein, albumin, LDH, triglycerides, cholesterol |
|
Ghodrati 2016 [40] |
Iran |
12 |
F |
Dyspnea, respiratory distress |
Chest trauma during play at school |
Bilateral |
N/A |
N/A |
N/A |
|
Lee 2016 [41] |
South Korea |
50 |
M |
Paraplegia |
Fall from height during construction work |
Right |
>1000-2000 |
3 |
Triglycerides |
|
Sendama 2015 [42] |
UK |
84 |
F |
Dyspnea, abnormal auscultation |
Fall |
Right |
500-1000 |
4 |
Protein, LDH, cholesterol, triglycerides |
|
Snow 2015 [43] |
USA |
22 months |
M |
Cough, dyspnea, respiratory distress, altered mental status, abnormal auscultation |
Fall from a chair |
Right |
<500 |
2 |
Triglycerides |
|
Adams 2013 [44] |
USA |
73 |
M |
Paraplegia, rib fractures, hemothorax |
RTA |
Right |
N/A |
9 |
Triglycerides, lymphocytes, glucose, LDH, lipemia |
|
Kumar 2013 [45] |
India |
32 |
M |
Blunt injury, fracture of right femur |
RTA |
Right |
>1000-2000 |
2 |
Triglycerides, chylomicrons |
|
23 |
M |
Hemopneumothorax, multiple rib fractures, subcutaneous emphysema |
RTA |
Right |
500-1000 |
1 |
Triglycerides |
||
|
40 |
M |
Hemothorax |
RTA |
Right |
500-1000 |
2 |
Triglycerides |
||
|
Sharkey 2012 [46] |
UK |
50 |
M |
Multiple fractures, hematoma, hemothorax, pneumothorax |
RTA |
Right |
500-1000 |
N/A |
Triglyceride, cholesterol |
|
Sokouti, 2011[30] |
Iran |
15 |
M |
Respiratory distress, dyspnea, back pain, abnormal auscultation |
Fall 11 years ago |
Bilateral |
>2000 |
40 |
Triglycerides, protein, cholesterol, fat |
|
Kurklinsky 2011 [47] |
USA |
26 |
F |
Pleuritic chest pain |
Water-skiing fall |
Bilateral |
>1000-2000 |
2 |
Triglycerides |
|
Apostolakis, 2009 [8] |
USA |
75 |
F |
Dyspnea, back pain |
RTA |
Bilateral |
500-1000 |
At once |
Protein, LDH, glucose, amylase, triglycerides, cholesterol, albumin, globulin, K, Na, lymphocytes, erythrocytes |
|
22 |
M |
Back pain, hematoma of left thigh, chest pain |
RTA |
Bilateral |
<500 |
0.25 |
Protein, LDH, glucose, amylase, triglycerides, cholesterol, albumin, globulin, K, Na, lymphocytes, erythrocytes |
||
|
Huber, 2009 [16] |
USA |
47 |
M |
Dyspnea, chest pain |
Crushed by multiple metal gates |
Bilateral |
500-1000 |
3 |
Triglycerides |
|
Schurz, 2009 [28] |
Austria |
39 |
M |
Dyspnea, thoracodorsal pain |
RTA |
Left |
>1000-2000 |
14 |
N/A |
|
Serin-Ezer, 2009 [29] |
Turkey |
4 |
M |
Dyspnea, somnolence, abnormal auscultation |
Hit by a manufacturing pipe falling from a truck |
Bilateral |
<500 |
At once |
Triglycerides, cholesterol, protein, LDH, glucose |
|
Kamiyoshihara, 2008 [18] |
Japan |
51 |
M |
Dyspnea, dullness in percussion |
RTA 20 years before presentation |
Bilateral |
>1000-2000 |
At once (but the trauma dated back to 20 years prior)
|
Triglycerides |
|
Pandey 2008 [48] |
Australia |
36 |
M |
Chest pain, flail chest, hypotension |
Fall from balcony |
Right |
>1000-2000 |
2 |
N/A |
|
Lee, 2006 [20] |
South Korea |
11 |
M |
Dyspnea, nausea, vomiting, abdominal discomfort, abnormal auscultation |
RTA 3 days before presentation |
Bilateral |
N/A |
3 |
Triglycerides, cholesterol, protein |
|
Ozcelik, 2004 [26] |
Turkey |
15 |
F |
Respiratory distress, subcutaneous emphysema, pneumothorax |
Trapping under rubble during a 7.8 magnitude earthquake |
Right |
N/A |
45 |
Cholesterol, triglycerides |
|
Robbins 2004 [49] |
USA |
41 |
M |
Chest injury, refractory hiccups, nausea |
RTA |
Bilateral |
N/A |
N/A |
N/A |
|
Buchan 2001 [50] |
UK |
18 |
M |
Dyspnea |
RTA |
Right |
>1000-2000 |
4 |
N/A |
|
Chamberlain, 2000 [11] |
UK |
29 |
M |
Pneumothorax, abdominal and paraspinal pain, loss of motor power, and sensation below T12/L1 |
RTA |
Right |
>1000-2000 |
0.88 |
N/A |
|
Glyn-Jones 2000 [51]
|
UK |
28 |
M |
Dyspnea, polytrauma, tachypnea |
RTA |
Left |
>2000 |
N/A |
Triglyceride, cholesterol, WBC |
|
Golden, 1999 [15] |
USA |
53 |
F |
Chest pain, multiple fractures, hemopneumothorax, abnormal auscultation |
RTA |
Left |
>2000 |
6 |
Triglycerides |
|
McCormick, 1999 [24] |
USA |
46 |
M |
Chest pain, dyspnea, abnormal auscultation, dullness to percussion |
Hit-and-run motor vehicle accident |
Bilateral |
>1000-2000 |
14 |
Protein, cholesterol, triglycerides |
|
Ikonomidis, 1997 [17] |
Canada |
17 |
M |
Closed head injury, multiple fractures, respiratory distress, tracheal hematoma |
RTA |
Bilateral |
<500 |
At once |
Triglycerides |
|
24 |
M |
Closed head injury, rib fractures, hemothorax |
Snowboarding accident |
Left |
<500 |
At once |
Triglycerides |
||
|
Guleserian, 1996 [52] |
USA |
11 months |
M |
Dyspnea, coughing, cold symptoms, grunting, abnormal percussion |
Child abuse |
Right |
500-1000 |
N/A |
Triglycerides, cholesterol, WBC |
|
Milano, 1994 [25] |
Italy |
26 |
F |
Dyspnea |
Fall while skiing 4 months prior |
Left |
>1000-2000 |
50 |
Triglycerides |
|
Fogli, 1993 [53] |
Italy |
31 |
M |
Suspected traumatic hemothorax, dyspnea, cough |
RTA |
Right |
500-1000 |
N/A |
N/A |
|
Grant, 1991 [54] |
New Zealand |
32 |
M |
Dyspnea, chest and back pain |
RTA |
Right |
>1000-2000 |
N/A |
N/A |
|
Dulchavsky, 1988 [13] |
USA |
48 |
M |
Dyspnea, chest pain, abnormal auscultation |
Fistfight |
Right |
>1000-2000 |
At once |
Cholesterol, HDL, triglycerides, pre-beta lipoprotein, chylomicrons |
|
Brook 1988 [55] |
USA |
27 |
M |
Respiratory distress, abnormal percussion, tachycardia |
RTA |
Bilateral |
>2000 |
3 |
Triglycerides
|
|
Pai, 1984 [27] |
USA |
19 |
M |
Neck, back, and chest pain |
RTA |
Right |
>1000-2000 |
N/A |
N/A |
|
Krishnan 1982 [56] |
Malaysia |
29 |
M |
Dyspnea, abnormal percussion |
RTA |
Right |
>2000 |
2 |
N/A |
|
Azambuja 1981 [57] |
Brazil |
42 |
M |
Paraplegia, hemopneumothorax |
RTA |
Right |
N/A |
3 |
N/A |
|
Rea 1960 [58] |
UK |
28 |
M |
Dyspnea, apex beat displaced to the left |
Crush injury from falling planks |
Right |
500-1000 |
4 |
Lipid, protein, RBC, lymphocytes |
|
Guest 1955 [59] |
Canada |
19 |
M |
Dyspnea, dry cough, tachypnea, dull percussion |
RTA |
Right |
>1000-2000 |
26 |
N/A |
|
Elliot 1948 [60] |
Canada |
56 |
M |
Fall injury, paraplegia, respiratory distress |
Fall from a tree |
Right |
500-1000 |
3 |
Fat |
|
Dorsey 1942 [61] |
USA |
60 |
M |
Alcoholic stupor, dyspnea, chest pain, abnormal percussion |
Fall down a flight of stairs |
Right |
>2000 |
0.5 |
Protein, albumin, globulin, fat |
|
Cellan-Jones 1940 [62] |
UK |
32 |
M |
Dyspnea, chest tightness |
A stone hitting the chest and dorsal spine striking a block of coal |
Right |
>1000-2000 |
3 |
Fat |
|
Brown 1937 [63] |
USA |
N/A |
F |
Respiratory distress, abdominal distention |
RTA |
Bilateral |
>1000-2000 |
At once |
N/A |
|
Bauersfeld 1937 [64] |
USA |
22 |
M |
Breathing difficulty, laceration of the scalp, pain in lower abdomen and lumbar region, cyanosis, cold extremities |
RTA |
Right |
>2000 |
8 |
Fat globules |
|
Lillie 1935 [65] |
USA |
45 |
M |
Blunt injury |
Fall from a scaffold 20 feet high |
Right |
>2000 |
N/A |
N/A |
|
Macnab 1932 [66] |
Canada |
46 |
M |
Chest and back pain, dullness percussion, dyspnea, anorexia, weakness, intermittent fever, hypotension |
Fall from a height of 11 feet |
Right |
500-1000 |
6 |
N/A |
|
F: female, M: male, CFP: clinical findings & presentation, SOC: Side of chylothorax, hr: hour, N/A: non-available, COAP: Chyle onset after presentation, RTA: road traffic accident, RBC: red blood cell, LDH: lactate dehydrogenase, HDL: high density lipoprotein, WBC: white blood cell. * The amount of chyle has been grouped rather than the actual amount. |
|||||||||
|
First author, year [Reference] |
Chest X-ray |
CT |
MRI |
ICU admission |
Treatment |
Thoracic duct ligation approach |
Mode of drainage |
Duration of chest tube placement (day) |
Follow-up (weeks) |
Outcome |
|
Harvey, 2024 [5] |
Pleural effusion |
Hemopneumothorax, pneumomediastinum, retrosternal hematoma, multiple rib fracture, lung contusions, and manubrium fractures |
N/A |
Yes |
Drainage, medium chain fatty acid diet |
N/A |
Chest tube |
7 |
8 |
Recovered |
|
Burduniuc, 2023 [2] |
Pleural effusion, multiple rip fracture |
Pleural effusion, multiple rib fracture |
Th12 vertebral fracture |
Yes |
Drainage, thoracic duct ligation |
Thoracotomy |
Chest tube |
N/A |
N/A |
Recovered |
|
Dung, 2023 [14] |
Pleural effusion |
T9 and T10 vertebral fracture |
N/A |
No |
Drainage, octreotide, TPN, thoracic duct embolization |
2.7 Fr microcatheter, fluoroscopic guidance |
Chest tube |
7 |
N/A |
Recovered |
|
Kim, 2023 [4] |
Pleural effusion |
Lipiodol leakage near T10–11 level |
N/A |
Yes |
Drainage, TPN, intranodal lymphangiography, therapeutic lipiodol injection |
N/A |
Chest tube |
39 |
N/A |
Recovered |
|
Boateng 2023 [33] |
N/A |
Pleural effusion, lung collapse |
N/A |
No |
Drainage, medium-chain triglyceride |
N/A |
Chest tube |
N/A |
N/A |
Died |
|
Ruest 2023 [34] |
Pleural effusion |
T12 vertebral body fracture, rib fractures |
N/A |
Yes |
Drainage |
N/A |
Chest tube |
N/A |
N/A |
Recovered |
|
Mohanakrishnan 2022 [35] |
N/A |
Pleural effusion, minimal ascites |
N/A |
No |
Drainage, octreotide, low-fat diet, NPO, TPN, pleurodesis, thoracic duct embolization |
Coiling and glue embolization |
Chest tube |
N/A |
N/A |
Recovered |
|
Mazhar, 2021[23] |
Pleural effusion |
Pleural effusion, T10 spinous process fracture |
N/A |
No |
Drainage, octreotide, medium-chain triglyceride diet |
N/A |
Chest tube |
3 |
N/A |
Recovered |
|
Waseem, 2021[32] |
Pleural effusion |
Pleural effusion |
N/A |
No |
Only drainage |
N/A |
Chest tube |
5 |
N/A |
Recovered |
|
Din Dar 2021 [36] |
N/A |
Multiple rib fractures, hemothorax |
N/A |
No |
Drainage, NPO, TPN, octreotide, thoracic duct embolization |
Thoracotomy |
Chest tube |
25 |
48 |
Recovered |
|
Bacon, 2020 [9] |
Multiple rib fracture |
Multiple rib fracture |
N/A |
Yes |
Drainage, free-fat diet |
N/A |
Chest tube |
N/A |
12 |
Recovered |
|
Champion, 2020 [12] |
Pleural effusion |
Pleural effusion |
N/A |
No |
Drainage, octreotide, TPN, thoracic duct ligation |
Thoracotomy |
Chest tube |
N/A |
6 |
Recovered |
|
Jindal 2019 [37] |
Pleural effusion |
Multiple rib fractures, lung contusions, fracture of L1 and L2 vertebrae |
N/A |
Yes |
Drainage, thoracic duct ligation, TPN, octreotide, fat-free and medium chain triglyceride |
Thoracotomy |
Chest tube |
8 |
8 |
Recovered |
|
Ahmed, 2018 [1] |
Opacification of hemithorax |
D10 vertebral fracture, multiple rib fracture |
N/A |
Yes |
Drainage, low-fat diet, albumin vial, octreotide |
N/A |
Chest tube |
|
|
|
|
Brown, 2018 [10] |
N/A |
Left temporal epidural hematoma, pulmonary contusions, multiple skeletal fractures, pneumomediastinum compressing the right atrium |
Not mentioned the findings |
No |
Drainage, NPO, TPN, octreotide, thoracic duct embolization, and ligation |
Thoracotomy, decortication |
Chest tube |
|
|
|
|
Litzau, 2018 [22] |
Pleural effusion |
Pleural effusion |
N/A |
No |
Drainage, low-fat diet |
N/A |
Chest tube |
|
|
|
|
Kozul, 2017 [19] |
N/A |
Hemopneumothorax, mediastinal shift to the right, pleural effusion |
N/A |
No |
Drainage, No fat/low-fat diet |
N/A |
Chest tube |
|
|
|
|
Lee, 2017 [21] |
Pleural effusion |
Multiple rib fracture, hemopneumothorax (left), subcutaneous emphysema (left), and atelectasis (right). |
N/A |
Yes |
Drainage, TPN, NPO, fat-free diet, medium-chain lipid diet, thoracic duct ligation, pleurectomy |
Thoracotomy |
Chest tube |
|
|
|
|
Mohamed, 2017 [3] |
Obliteration of left costophrenic angle (pleural effusion) |
Bilateral effusion |
N/A |
No |
Drainage, fat-free diet with medium-chain triglycerides, octreotide |
N/A |
Thoracentesis |
|
|
|
|
Spasić, 2017 [6] |
Lung contusion |
Rib and thoracic vertebral fracture, hydropneumothorax, lung contusion, pneumomediastinum |
N/A |
No |
Drainage, TPN, thoracic duct suturing |
Thoracotomy |
Chest tube |
|
|
|
|
Sriprasit, 2017 [31] |
N/A |
N/A |
N/A |
Yes |
Drainage, NPO, TPN |
N/A |
Chest tube |
|
|
|
|
Hara 2017 [38] |
Pleural effusion |
N/A |
N/A |
No |
Drainage, low-fat diet with medium-chain triglycerides, intranodal lymphangiography with lipiodol |
N/A |
Chest tube |
|||
|
Jahn 2017 [39] |
Pulmonary opacification |
Lung contusions |
N/A |
No |
Drainage, fat-free diet |
N/A |
Chest tube |
|||
|
Ghodrati 2016 [40] |
Pleural effusion |
N/A |
N/A |
Yes |
Drainage, thoracic duct embolization |
Unknown |
Chest tube |
|||
|
Lee 2016 [41] |
N/A |
Incomplete cord injury at the thoracic spinal vertebrae (T10 and T11) |
N/A |
No |
Drainage, TPN, NPO, thoracic duct ligation |
VATS |
Chest tube |
|||
|
Sendama 2015 [42] |
Pleural effusion |
Multisegment fracture of L1 vertebra |
N/A |
No |
Drainage, medium chain fatty acid diet, octreotide |
N/A |
Chest tube |
|||
|
Snow 2015 [43] |
Opacification of right chest, mediastinal shift to left |
N/A |
N/A |
Yes |
Drainage, NPO, TPN, octreotide, low-fat diet |
N/A |
Chest tube |
|||
|
Adams 2013 [44] |
Pleural effusion, atelectasis |
Pleural effusion, atelectasis |
N/A |
Yes |
Drainage, NPO, TPN, octreotide |
N/A |
Thoracentesis, chest tube |
|||
|
Kumar 2013 [45] |
N/A |
Pleural effusion, multiple rib fractures |
N/A |
No |
Drainage, NPO, TPN, octreotide, chest physiotherapy |
N/A |
Chest tube |
|||
|
N/A |
Hemopneumothorax, multiple rib fractures |
N/A |
No |
Drainage, NPO, TPN, octreotide, chest physiotherapy |
N/A |
Chest tube |
||||
|
N/A |
Bilateral hemothorax, lung contusion |
N/A |
Yes |
Drainage, NPO, TPN, octreotide, exploratory laparotomy for biliary leak |
N/A |
Chest tube |
||||
|
Sharkey 2012 [46] |
N/A |
N/A |
N/A |
Yes |
Drainage, NPO, TPN, octreotide, medium fatty acid diet |
N/A |
Chest tube |
|||
|
Sokouti, 2011[30] |
Large cystic mass in left posterior mediastinum |
Large low-density cystic mass in the left posterior mediastinum, left pleural effusion |
N/A |
No |
Drainage, thoracic duct ligation, TPN |
Laparotomy, Thoracotomy |
Chest tube |
|||
|
Kurklinsky 2011 [47] |
N/A |
Pleural effusion, dilated cisterna chyli, middle mediastinum fluid collection |
N/A |
No |
Drainage, TPN, thoracic duct embolization |
3 Fr microcatheter with ultrasound guidance |
Thoracentesis |
|||
|
Apostolakis, 2009 [8] |
Pleural effusion |
Pleural effusion |
N/A |
No |
Drainage, starvation diet, TPN |
N/A |
Chest tube |
|||
|
Pleural effusion, rib fractures, ipsilateral sternoclavicular joint dislocation |
Lung contusion |
N/A |
No |
Drainage, starvation diet, TPN |
N/A |
Chest tube |
||||
|
Huber, 2009 [16] |
Pleural effusion |
Pleural effusion, right pneumothorax, multiple rib fracture, aortic pseudoaneurysm, retrocrural hemorrhage |
N/A |
Yes |
Drainage, thoracic duct ligation, medium chain fatty acid diet, mechanical pleurodesis |
Thoracotomy |
Chest tube |
|||
|
Schurz, 2009 [28] |
Multiple rib fracture, pleural effusion |
Pleural effusion |
Osseous lesions and pleural effusion |
Yes |
Drainage, TPN, fat-free diet, plain tea, apple puree |
N/A |
Pleural puncture, chest tube |
|||
|
Serin-Ezer, 2009 [29] |
Multiple rib fracture, pleural effusion |
Pleural effusion |
N/A |
No |
Drainage, NPO, TPN |
N/A |
Chest tube |
|||
|
Kamiyoshihara, 2008 [18] |
Pleural effusion |
Pleural effusion |
N/A |
No |
Drainage, low-fat diet, TPN, thoracic duct ligation, pleurodesis |
Thoracotomy |
Thoracentesis, Chest tube |
|||
|
Pandey 2008 [48] |
N/A |
Hemopneumothorax, pulmonary contusion, multiple rib fractures, pneumomediastinum |
N/A |
Yes |
Drainage, octreotide, thoracic duct ligation |
Laparoscopic ligation |
Chest tube |
|||
|
Lee, 2006 [20] |
Elevation of diaphragms, cardiomegaly |
Pleural effusion, massive ascites around liver and spleen |
N/A |
No |
Drainage, medium-chain lipid solution, NPO |
N/A |
Thoracentesis, chest tube |
|||
|
Ozcelik, 2004 [26] |
Pneumothorax, consolidated right lung, pleural effusion |
Right lung consolidation, pleural effusion |
N/A |
No |
Drainage, thoracic duct mass ligation, TPN |
Thoracotomy |
Chest tube |
|||
|
Robbins 2004 [49] |
N/A |
Pleural effusion, focal fluid collection |
N/A |
No |
EUS-guided aspiration, injection of sodium morrhuate |
N/A |
Aspiration |
|||
|
Buchan 2001 [50] |
Pleural effusion |
N/A
|
N/A |
No |
Drainage, low-fat diet, medium-chain triglycerides, thoracic duct ligation |
Thoracotomy |
Chest tube |
|||
|
Chamberlain, 2000 [11] |
Pneumothorax, hemithorax opacification |
Free abdominal gas |
Fractures of T4 and T10 with spinal cord contusion and hematoma |
No |
Drainage, TPN, NPO, Supradiaphragmatic duct ligation |
Thoracotomy |
Chest tube |
|||
|
Glyn-Jones 2000 [51]
|
Mediastinal shift |
Minor anterior wedge fractures at T5 and T10 |
Cord injury at T10 |
No |
Drainage, thoracic duct ligation, pleurodesis, fat-free diet |
Thoracotomy |
Chest tube |
|||
|
Golden, 1999 [15] |
N/A |
N/A |
N/A |
Yes |
Drainage, TPN, NPO, thoracic duct ligation |
Thoracotomy |
Chest tube |
|||
|
McCormick, 1999 [24] |
Pleural effusion |
Disruption of the thoracic duct at the T5 level |
N/A |
No |
Only drainage |
N/A |
Chest tube |
|||
|
Ikonomidis, 1997 [17] |
Pneumomediastinum, pulmonary contusions |
N/A |
N/A |
No |
Drainage, TPN, bowel rest |
N/A |
Chest tube |
|||
|
Left hemothorax |
Left mediastinal hematoma, T3 vertebral fracture |
N/A |
No |
Drainage, TPN, bowel rest |
N/A |
Chest tube |
||||
|
Guleserian, 1996 [52] |
Right lung opacification and mediastinal shift to left |
N/A |
N/A |
No |
Drainage, nasogastric feeding with medium-chain triglycerides, low-fat diet |
N/A |
Chest tube |
|||
|
Milano, 1994 [25] |
Pleural effusion |
Dense lymphatic opacification at L1-L2, chyloma at D11, pleural leakage from left duct |
N/A |
No |
Drainage, low-fat diet, medium-chain triglycerides, TPN, pleuroperitoneal shunt |
N/A |
Thoracentesis |
|||
|
Fogli, 1993 [53] |
Pleural effusion, mediastinal shift |
N/A |
N/A |
No |
Drainage, TPN |
N/A |
Chest tube |
|||
|
Grant, 1991 [54] |
Pleural effusion |
N/A |
N/A |
No |
Drainage, thoracic duct ligation, TPN, low-fat diet |
Thoracotomy |
Thoracocentesis, chest tube |
|||
|
Dulchavsky, 1988 [13] |
Pleural effusion |
N/A |
N/A |
No |
Drainage, TPN, NPO, thoracic duct ligation |
Thoracotomy |
Chest tube |
N/A |
144 |
Recovered |
|
Brook 1988 [55] |
Pleural effusion |
N/A |
N/A |
Yes |
Drainage, NPO, TPN, low-fat/ high-protein diet |
N/A |
Chest tube |
10 |
32 |
Recovered |
|
Pai, 1984 [27] |
Fracture dislocations of C6-C7 and T11-T12, right hemothorax |
N/A |
N/A |
No |
Drainage, fat-free diet, TPN, thoracic duct ligation, parietal pleurectomy |
Thoracotomy |
Chest tube |
N/A |
N/A |
Recovered |
|
Krishnan 1982 [56] |
Pleural effusion, obliteration of left costophrenic angle, multiple rib fractures |
N/A |
N/A |
No |
Drainage, thoracic duct ligation |
Thoracotomy |
Chest tube |
19 |
5 |
Recovered |
|
Azambuja 1981 [57] |
Hemopneumothorax |
N/A |
N/A |
No |
Drainage, thoracic duct ligation, pleural flap to address fistula, pleural abrasion |
Thoracotomy |
Chest tube |
6 |
N/A |
Recovered |
|
Rea 1960 [58] |
Opaque hemithorax |
N/A |
N/A |
No |
Drainage, thoracic duct ligation |
Thoracotomy |
Chest tube |
N/A |
N/A |
Recovered |
|
Guest 1955 [59] |
N/A |
N/A |
N/A |
No |
Aspiration, high-protein, low-fat diet |
N/A |
Thoracentesis |
N/A |
4 |
Recovered |
|
Elliot 1948 [60] |
Pleural effusion |
N/A |
N/A |
No |
Aspiration, thoracic duct ligation |
Thoracotomy |
Aspiration |
N/A |
N/A |
Recovered |
|
Dorsey 1942 [61] |
Rib fracture, pleural effusion |
N/A |
N/A |
No |
Drainage, low-fat diet, high-carb, high-protein diet, NPO |
N/A |
Thoracentesis |
N/A |
N/A |
Died due to uncontrolled leakage |
|
Cellan-Jones 1940 [62] |
Pleural effusion |
N/A |
N/A |
No |
Aspiration, low-fat diet, intravenous glucose-saline |
N/A |
Aspiration |
N/A |
N/A |
Died due to uncontrolled leakage |
|
Brown 1937 [63] |
Pleural effusion |
N/A |
N/A |
No |
Drainage, dietary management |
N/A |
Thoracentesis, paracentesis |
N/A |
N/A |
Died |
|
Bauersfeld 1937 [64] |
Pleural effusion, mediastinal shift |
N/A |
N/A |
No |
Drainage, intravenous dextrose, high-calorie diet |
N/A |
Thoracentesis |
16 |
N/A |
Recovered |
|
Lillie 1935 [65] |
Pleural effusion, mediastinal displacement |
N/A |
N/A |
No |
Drainage, fat-free diet |
N/A |
Thoracentesis |
N/A |
N/A |
Recovered |
|
Macnab 1932 [66] |
Displacement of the heart, pleural effusion |
N/A |
N/A |
No |
Drainage, carbohydrates, protein |
N/A |
Aspiration |
48 |
2 |
Died due to extreme asthenia |
|
CT: computed tomography, MRI: magnetic resonance imaging, ICU: intensive care unit, NPO: Nulla Per Os, TPN: total parenteral nutrition, N/A: non-available, EUS: endoscopic ultrasound |
||||||||||
Presentation and etiology
The patients ranged in age from 11 months to 84 years, with a mean of 37.4 ± 19.9 years. Most cases were male (73.91%), while females accounted for 26.09%. The most common presenting symptom or clinical findings were dyspnea, observed in 47.83% of cases, followed by abnormal findings on auscultation or percussion (34.78%) and multiple fractures or injuries (27.54%). Other frequent symptoms included chest pain (21.74%) and pneumothorax, hemothorax, or hemopneumothorax (20.29%). Road traffic accidents (RTA) were the most prevalent cause of BCTC, accounting for 59.42% of cases, followed by falls (23.19%), trauma caused by heavy objects (8.70%), physical punishment or child abuse (4.34%), and fistfights (1.45%). Bilateral chylothorax was observed in 27.54% of cases, while 55.07% had right-sided involvement and 17.39% had left-sided involvement. The chyle leakage ranged widely, which was >1000–2000 mL/day in 40.58% of cases. Smaller volumes (<500 mL/day) were noted in 14.50% and 500 – 1000 mL/day in 20.28%. In 14.50% of cases, >2000 mL/day was drained. Chyle onset occurred within two days of presentation in 40.58% of cases and within three days to a week in 31.88%. Delayed onset (beyond one week) was reported in 13.04% of cases. The chyle predominantly contained only lipids (40.57%). Other compositions included lipid-protein mixtures (11.59%) and lipid-inflammatory cells (7.24%). Complex mixtures of lipids, proteins, sugars, inflammatory cells, and ions were seen in smaller proportions (5.80%) (Table 3).
|
Variables |
Frequency / Percentage |
|
Patient demography |
|
|
Age range (mean ± SD), years |
11 months – 84 (37.4 ± 19.9) |
|
Gender Male Female |
51 (73.91%) 18 (26.09%) |
|
Common presentation and clinical findings* Dyspnea Abnormal auscultation or percussion Multiple fractures or injuries Chest pain Pneumothorax/ hemothorax/ hemopneumothorax Back pain Respiratory distress |
33 (47.83%) 24 (34.78%) 19 (27.54%) 15 (21.74%) 14 (20.29%) 11 (15.94%) 11 (15.94%) |
|
Cause of blunt trauma Road traffic accident Fall Hit or crushed by heavy objects Physical punishment & child abuse Fistfight Others |
41 (59.42%) 16 (23.19%) 6 (8.70%) 3 (4.34%) 1 (1.45%) 2 (2.90%) |
|
Side of chylothorax Right Left Bilateral |
38 (55.07%) 12 (17.39%) 19 (27.54%) |
|
Amount of chyle (ml/day) <500 500 - 1000 >1000-2000 >2000 N/A |
10 (14.50%) 14 (20.28%) 28 (40.58%) 10 (14.50%) 7 (10.14%) |
|
Chyle onset after presentation (day) At once – 2 days 3 days – one week > one week – one month > one month N/A |
28 (40.58%) 22 (31.88%) 6 (8.70%) 3 (4.34%) 10 (14.50%) |
|
Biochemical content of chyle Lipid Lipid + Protein Lipid + Inflammatory cells Lipid + Protein + Sugar + Inflammatory cells + Ions Lipid + Protein + Sugar Lipid + Inflammatory cells + Protein N/A |
28 (40.57%) 8 (11.59%) 5 (7.24%) 4 (5.80%) 2 (2.90%) 2 (2.90%) 20 (29.00%) |
|
Imaging findings |
|
|
Chest X-rays* Pleural effusion Rib Fracture Lung/ mediastinal/ heart shift Opacification of lung Pneumothorax/ hemothorax Lung contusion Pneumomediastinum Vertebral fracture Lung consolidation Others N/A |
38 (55.07%) 7 (10.14%) 7 (10.14%) 6 (8.70%) 5 (7.24%) 2 (2.90%) 1 (1.45%) 1 (1.45%) 1 (1.45%) 5 (7.24%) 15 (21.74%) |
|
CT scan findings* Pleural effusion Rib fracture Vertebral fracture Pneumothorax/ hemothorax/ hemopneumothorax Lung contusion Pneumomediastinum Hematoma Thoracic duct leakage Others N/A |
23 (33.33%) 14 (20.29%) 10 (14.50%) 9 (13.04%) 8 (11.59%) 4 (5.80%) 3 (4.34%) 2 (2.90%) 17 (24.64%) 25 (36.23%) |
|
ICU admission Yes No |
19 (27.54%) 50 (72.46%) |
|
Common treatment approach* Drainage Parenteral nutrition Thoracic duct ligation/embolization/suturing Medium-chain fatty acid or low-fat diet Nulla per Os Free fat diet/starvation diet Octreotide Pleurectomy/Pleurodesis |
65 (94.20%) 35 (50.72%) 27 (39.13%) 24 (34.78%) 19 (27.54%) 12 (17.39%) 17 (24.64%) 6 (8.70%) |
|
Thoracic duct closure approach Thoracotomy Fr microcatheter with fluoroscopic/ ultrasound guidance VATS/ laparoscopy Coiling and glue embolization Unknown Not performed |
22 (31.88%) 2 (2.90%) 2 (2.90%) 1 (1.45%) 1 (1.45%) 41 (59.42%) |
|
Mode of drainage Chest tube Thoracentesis Aspiration Chest tube + Thoracentesis |
53 (76.81%) 9 (13.04%) 4 (5.80%) 3 (4.34%) |
|
Duration of chest tube placement ≤ One week > One week – two weeks > Two weeks – one month > One month N/A |
12 (17.39%) 11 (15.94%) 13 (18.84%) 4 (5.80%) 29 (42.03%) |
|
Outcome Recovered Partially recovered Died |
62 (89.85%) 1 (1.45%) 6 (8.70%) |
|
SD: standard deviation, CT: computed tomography, ICU: intensive care unit, VATS: video-assisted thoracoscopic surgery, N/A: non-available. *Each data in the variable might be found in more than one case |
|
Imaging characteristics and management
Chest X-rays revealed pleural effusion in 55.07% of cases, rib fractures, and lung or mediastinal or heart shift, each in 10.14%, lung opacification in 8.70%, and pneumothorax or hemothorax in 7.24%. Computed tomography (CT) scans confirmed pleural effusion in 33.33% and rib fractures in 20.29%. The vertebral fracture was found in 14.50%, and pneumothorax, hemothorax, or hemopneumothorax in 13.04%. Drainage was performed in 94.20%, predominantly via chest tubes (76.81%). In 17.39% of patients, the chest tube was in place for one week or less, while 15.94% required chest tube placement for more than one week until two weeks. Another 18.84% needed chest tube placement for over two weeks to one month, and 5.80% had chest tube placement exceeding one month. Additional treatments included parenteral nutrition (50.72%), thoracic duct closure (39.13%), and dietary modifications such as a medium-chain fatty acid or low-fat diet (34.78%). Pharmacological treatments included octreotide in 24.64% of cases. Thoracic duct closure was performed through thoracotomy in 31.88%. Other less-used techniques included Fr microcatheter under radiological guidance in 2.90%, video-assisted thoracoscopy or laparoscopy in 2.90%, and coiling and glue embolization in 1.45%. In 59.42% of cases, thoracic duct closure was not performed. The majority of patients (89.85%) achieved complete recovery, with one case showing partial recovery (1.45%), and six cases died (8.70%) (Table 3).
Discussion
Chylothorax is a pathological condition; if left untreated, it can result in respiratory distress and various complications. The etiology is multifaceted, including traumatic causes, while non-traumatic factors may involve conditions that elevate lymphatic pressure or cause obstruction, such as lymphoma or heart failure [1,67]. Chylothorax was first documented in the medical literature during the 19th century but has since garnered increasing recognition with advancements in diagnostic and surgical techniques. Improved imaging modalities and surgical innovations have significantly enhanced the understanding of its pathophysiology, facilitating more effective identification and management of its underlying causes [1,2].
The demographic data in the present review revealed an age range of 11 months to 84 years, with a mean age of 37.4 ± 19.9 years. This aligns with the literature, as Elsaied et al. reported an approximate mean age of 42.67 years within an age range of 18 to 76 years [68]. Case reports have identified young adults as particularly susceptible to chylothorax following blunt chest trauma, who are commonly involved in motor vehicle collisions or sports injuries [12,31]. Conversely, another study found that individuals aged 50 years or older represented the most common age group among blunt chest trauma patients, comprising 28.9% of the sample [69]. This reflects the increased risk of falls and accidents among older populations [70]. The slightly lower mean age in the present study may be attributable to the inclusion of pediatric cases, broadening the demographic scope. A significant male predominance was observed in the current review, with 73.91% of cases involving males. This finding concurs with the literature, where male representation ranged from 72.3% in a literature review [71] to 85.4% in a cohort study on blunt chest trauma cases [69]. This gender disparity is often linked to higher exposure to high-risk activities and occupations among males [12,31].
The clinical presentation of chylothorax is variable, with dyspnea being the most common symptom, reported by approximately 66.7% of patients. Dyspnea arises from fluid accumulation in the pleural space, which restricts lung expansion and impairs gas exchange. Patients may also experience a dry cough, often exacerbated by pleural fluid [72]. Pleuritic chest pain is another potential symptom, likely caused by pleural irritation from chyle [3,5]. On physical examination, percussion of the thorax often reveals dullness over the affected area due to fluid accumulation, contrasting with the typical resonance of healthy lung tissue [3,12,22]. Auscultation typically shows diminished or absent breath sounds over regions where fluid has accumulated, reflecting impaired air movement [72]. In this review, consistent with the literature, dyspnea was the most common presenting symptom (47.83%). This was followed by abnormal findings on auscultation or percussion in 34.78% of cases. Other frequently reported symptoms included chest pain (21.74%) and complications such as pneumothorax, hemothorax, or hemopneumothorax (20.29%).
The thoracic duct, the primary conduit for lymphatic fluid, can be ruptured or injured by blunt trauma, leading to chyle leakage into the pleural space [71,73]. Damage to adjacent structures, such as vertebral fractures or mediastinal injuries, can also contribute to chylothorax. For example, thoracic spine injuries have been associated with chylothorax due to their anatomical proximity to the thoracic duct [4,14]. Chylothorax is predominantly unilateral. In a study of 74 cases, 78% involved one hemithorax, with the right side being affected in 67% and the left in 33%. Bilateral pleural effusion was observed in 22% of cases [74]. The volume of chyle leakage varies based on the severity of the injury and the extent of thoracic duct damage. Low-output chylothorax (<1000 mL/day) is typically managed conservatively, whereas high-output cases (>1–1.5 L/day) often require surgical or radiological intervention [4,37,75]. In extreme cases, chyle output exceeding 2000 mL/day has been reported [6,15,21,30]. Blunt chest trauma frequently results from RTA, underscoring the risks of high-speed collisions [5,22,32]. Falls are another common cause, accounting for approximately 45% of cases in a study of patients with multiple traumas [76]. In this review, RTA was found to be the leading cause of injury in 41 cases (59.42%), followed by falls in 16 cases (23.19%), trauma by heavy objects in 6 cases (8.70%), physical punishment or child abuse in three cases (4.34%) and fistfights in one case (1.45%). Bilateral chylothorax occurred in 27.54% of cases, higher than previously reported. Consistent with the literature, right-sided involvement (55.07%) was more common than left-sided involvement (17.39%). This finding contrasts with the observation of Kakamad et al., who reported no laterality difference, but is similar to the findings of Maldonado et al., who reported right-sided involvement in 67% of cases and left-sided involvement in 33% [71,74]. Chyle volume varied significantly, with 40.58% of cases producing >1000–2000 mL/day, while 10 cases (14.50%) exceeded 2000 mL/day.
The timing of chyle onset in this review varied, with symptoms developing within two days in 40.58% of cases and within three days to a week in 31.88%. These align with the finding that chylothorax most commonly manifests within 2 to 7 days following blunt chest trauma due to gradual pleural accumulation from duct leakage [71]. However, delayed onset beyond one month, as observed in 4.34% of reviewed cases, is rare but documented in the literature, with an extreme case reported up to 20 years post-trauma [18]. The biochemical composition of chyle among the reviewed cases primarily consisted of lipids (40.57%), with smaller proportions of lipid-protein mixtures (11.59%) and lipid-inflammatory cell mixtures (7.24%). Complex mixtures, including lipids, proteins, sugars, inflammatory cells, and ions, were identified in 5.80% of cases. These findings are consistent with the established biochemical profile of chyle, which is rich in triglycerides (≥110 mg/dL) and lymphocytes [71]. As reported in the literature, immunoglobulins and protein levels ranging from 2.2 to 6 g/dL underscore the nutritional and immunological impact of chyle loss [1,8,32].
In the present review, chest X-rays revealed pleural effusion in 55.07% of cases, consistent with its status as the most common radiographic finding in chylothorax, typically presenting as a homogeneous opacity [2,4,32,71]. Rib fractures and lung or mediastinal or heart shift each were observed in 10.14% of cases, with lung opacification in 8.70% and pneumothorax, or hemothorax in 7.24%, aligning with literature that highlights the utility of chest X-rays in detecting associated traumatic injuries, such as rib fractures and pulmonary contusions [2,6,77]. CT scans in the reviewed cases showed pleural effusion in 33.33% of cases and rib fractures in 20.29%. The detection of pneumothorax, hemothorax, or hemopneumothorax in 13.04% of cases further emphasizes the role of CT in visualizing coexisting traumatic injuries with greater detail than X-rays [4,77].
The initial approach to managing chylothorax primarily involves conservative measures, including nil per os (nothing by mouth), total parenteral nutrition, and adherence to a low-fat diet. Pharmacological interventions, such as octreotide, may decrease lymphatic flow and facilitate the closure of the leak [10,14,21,23]. In chylothorax management, chest tube placement is commonly maintained until chyle drainage significantly decreases or resolves. The duration varies from a few days to several weeks, influenced by the effectiveness of conservative approaches [78]. In this review, the chest tube was in place for one week or less in 17.39% of patients, while 15.94% required chest tube placement for more than one week until two weeks. Another 18.84% needed chest tube placement for over two weeks to one month, and 5.80% had chest tube placement exceeding one month.
In cases where conservative management proves ineffective, surgical intervention becomes imperative. Thoracic duct ligation remains the definitive surgical option and can be performed via open thoracotomy or minimally invasive approaches [79]. Based on the findings of this review, besides drainage, treatments for chylothorax included parenteral nutrition (50.72%), thoracic duct closure (39.13%), and dietary modifications, such as a medium-chain fatty acid or low-fat diet (34.78%). Octreotide was administered in 24.64% of cases. Thoracic duct closure was performed via thoracotomy in 31.88% of cases, Fr microcatheter with fluoroscopic/ ultrasound guidance in 2.90%, VATS or laparoscopy in 2.90%, and coiling and glue embolization in 1.45%. In 59.42% of cases, thoracic duct closure was not performed or was unnecessary.
The limitations of this study include the inherent nature of the reviewed studies, which were exclusively case reports due to the rarity of the condition. Consequently, drawing conclusions based on statistical analyses was not feasible. Additionally, the small sample size and the non-standardized data reporting across the included reports may have introduced potential bias into the findings of this review. While every effort was made to include all relevant studies identified through the search using predefined keywords, there remains the possibility that some studies were inadvertently overlooked.
Conclusion
BCTC is rare and complex, underscored by the wide variability in patient demographics, clinical presentations, chylothorax onset, and management approaches. Given the challenges posed by limited evidence, the findings emphasize the need for early recognition and individualized management strategies.
Declarations
Conflicts of interest: The authors have no conflicts of interest to disclose.
Ethical approval: Not applicable.
Consent for participation: Not applicable.
Consent for publication: Not applicable.
Funding: The present study received no financial support.
Acknowledgements: None to be declared.
Authors' contributions: FHK and HOA: major contributors to the conception of the study, as well as the literature search for related studies, and manuscript writing. HKA, BJHA, and HMA: Literature review, critical revision of the manuscript, and processing of the tables. SHM, BeAA, SMA, MNH, SSA, YMM, KAN, SHK and BaAA: Data extraction, data organization, and critical revision. All authors have read and approved the final version of the manuscript.
Use of AI: ChatGPT-3.5 was used to assist with language refinement and improve the overall clarity of the manuscript. All content was thoroughly reviewed and approved by the authors, who bear full responsibility for the final version.
Data availability statement: Not applicable.
References
- Ahmed OF, Kakamad FH, Mohammed SH, Aziz MS. Blunt chest trauma causing chylothorax: A case report with literature review. 2018; 5(2):100015C04OA2018. doi:10.5348/100015C04OA2018CR
- Burduniuc A, Habal P. Blunt chest injury with chylothorax and thoracic vertebral fracture-multidisciplinary management. Arta Medica. 2023;87(2):138-41. doi:10.5281/zenodo.8213294
- Mohamed M, Alshenawy W, Kegarise C, Betten D. Bilateral chylothorax due to blunt trauma without radiographic evidence of traumatic injury. Clinical practice and cases in emergency medicine. 2017;1(2):111. doi:10.5811/cpcem.2016.12.32937
- Kim G, Noh D, Kim BM, Heo Y. Delayed Chylothorax Following Blunt Chest Trauma Treated with Repeated Lymphangiography: A Case Presentation. Journal of Acute Care Surgery. 2023;13(1):39-42. doi:10.17479/jacs.2023.13.1.39
- Harvey C, Shin H, Martin S, Perea L. Traumatic chylothorax following blunt thoracic trauma. Trauma Case Reports. 2024; 54:101101. doi:10.1016/j.tcr.2024.101101
- Spasic M, Arsenijević M, Dončić N, Mrvić S, Stojkovic D, Milosevic B, et al. A rare case of traumatic chylothorax after blunt thoracic trauma.2017;145(1-2):73-76. doi:10.2298/SARH160218015S
- Abdullah HO, Abdalla BA, Kakamad FH, Ahmed JO, Baba HO, Hassan MN, et al. Predatory publishing lists: a review on the ongoing battle against fraudulent actions. Barw Medical Journal. 2024; 2(2):26-30. doi:10.58742/bmj.v2i2.91
- Apostolakis E, Akinosoglou K, Koletsis E, Dougenis D. Traumatic chylothorax following blunt thoracic trauma: two conservatively treated cases. Journal of cardiac surgery. 2009;24(2):220-2. doi:10.1111/j.1540-8191.2009.00828.x
- Bacon BT, Mashas W. Chylothorax caused by blunt trauma: case review and management proposal. Trauma Case Reports. 2020; 28:100308. doi:10.1016/j.tcr.2020.100308
- Brown SR, Fernandez C, Bertellotti R, Asensio JA. Blunt rupture of the thoracic duct after severe thoracic trauma. Trauma surgery & acute care open. 2018;3(1): e000183. doi:10.1016/j.tcr.2020.100308
- Chamberlain M, Ratnatunga C. Late presentation of tension chylothorax following blunt chest trauma. European Journal of cardio-thoracic Surgery. 2000;18(3):357-9. doi:10.1016/S1010-7940(00)00532-7
- Champion S, Cheung VL, Wiseman D. Isolated thoracic duct injury from blunt force trauma. Journal of Radiology Case Reports. 2020;14(9):18. doi:10.3941/jrcr.v14i9.3977
- Dulchavsky SA, Ledgerwood AM, Lucas CE. Management of chylothorax after blunt chest trauma. Journal of Trauma and Acute Care Surgery. 1988;28(9):1400-1. doi:10.1097/00005373-198809000-00018
- Dung LT, Van Sy T, Linh NT, Tuyen DT, Hung DT, Van Cuong V, et al. Successful treatment of thoracic duct injury from blunt trauma. Radiology Case Reports. 2023;18(6):2121-5. doi:10.1016/j.radcr.2023.02.061
- Golden P. Chylothorax in blunt trauma: a case report. American Journal of Critical Care. 1999;8(3):189.
- Huber N, Giglia J, Starnes S, Tsuei B. Concomitant blunt aortic and thoracic duct injury. Injury Extra. 2009;40(5):81-3. doi:10.1016/J.INJURY.2009.01.004
- Ikonomidis JS, Boulanger BR, Brenneman FD. Chylothorax after blunt chest trauma: a report of 2 cases. Canadian journal of surgery. 1997;40(2):135.
- Kamiyoshihara M, Ibe T, Kakegawa S, Sato K, Takise A, Takeyoshi I. Late-onset chylothorax after blunt chest trauma at an interval of 20 years: report of a case. Surgery today. 2008; 38:56-8. doi:10.1007/s00595-007-3557-x
- Kozul C, Jassal K, Judson R. Massive bilateral chylothorax post blunt trauma. Trauma case reports. 2017; 12:63-5. doi:10.1016/j.tcr.2017.10.024
- Lee SB, Lee SH, Kim JH, Lee JY, Si JW, Do BS. A Case of Chylothorax after Blunt Chest Trauma Accompanied by Nephrotic Syndrome. KSEM. 2006;17(6):659.
- Lee J, Cho JS, I H, Kim YD. Delayed right chylothorax after left blunt chest trauma: a case report. Journal of Medical Case Reports. 2017; 11:1-5. doi:10.1186/s13256-017-1250-2
- Litzau M, Welch JL. Chylothorax after blunt trauma.2018; 10: 58-9. doi:10.3978/j.issn.2072-1439.2011.09.03
- Mazhar K, Mohamed S, Patel AJ, Berger-Veith S, Abid Q, Ghosh S. Delayed chylothorax in the absence of radiological evidence of rib or vertebral body fractures following blunt trauma. Journal of Surgical Case Reports. 2021;2021(4):rjab112. doi:10.1093/jscr/rjab112
- McCormick III J, Henderson SO. Blunt trauma-induced bilateral chylothorax. The American Journal of Emergency Medicine. 1999;17(3):302-4. doi:10.1016/s0735-6757(99)90130-4
- Milano S, Maroldi R, Vezzoli G, Bozzola G, Battaglia G, Mombelloni G. Chylothorax after blunt chest trauma: an unusual case with a long latent period. The Thoracic and cardiovascular surgeon. 1994;42(03):187-90. doi:10.1055/s-2007-1016485
- Ozcelik C, Onat S, Bayar ES. Combined late diagnosed right main bronchial disruption and chylothorax from blunt chest trauma. The Annals of Thoracic Surgery. 2004 ;78(4):e61-2. doi:10.1016/j.athoracsur.2003.08.070
- Pai GP, Bhatti NA, Ellison RG, Rubin JW, Moore HV. Thoracic duct injury from blunt trauma. Southern Medical Journal. 1984;77(5):667-8. doi:10.1097/00007611-198405000-00037
- Schurz M, Petras N, Platzer P, Hofbauer F, Vécsei V. Delayed chylothorax following blunt chest trauma. European Journal of Trauma and Emergency Surgery. 2010; 36:76-80. doi:10.1007/s00068-009-8127-z
- Serin-Ezer S, Oğuzkurt P, İnce E, Hiçsönmez A. Bilateral chylothorax after blunt thoracic trauma: a case report. The Turkish Journal of Pediatrics. 2009;51(5):504-6.
- Sokouti M, Aghdam BA. Delayed concurrent chylothorax and chyloperitoneum: report of a case after an old blunt trauma. Tanaffos. 2011;10(1):52.
- Sriprasit P, Akaraborworn O. Chylothorax after blunt chest trauma: a case report. The Korean Journal of Thoracic and Cardiovascular Surgery. 2017;50(5):407. doi:10.5090/kjtcs.2017.50.5.407
- Waseem M, Rafiq M, Malik MH. Bilateral Chylothorax Post Blunt Trauma: A Case Report. Journal of Rawalpindi Medical College. 2021;25(4):578-80. doi:10.37939/jrmc.v25i4.1788
- Boateng HA, Wakeman A, Felek S. Traumatic chylothorax: a case report and literature review. CHEST. 2023;164(4): A3668. doi:10.1016/j.rmcr.2015.01.001
- Stephanie Ruest MD, Beucher M. A case of child abuse presenting with a traumatic chylothorax. Rhode Island Medical Journal. 2023;106(10):25-8.
- Mohanakrishnan BP, Tasnim S, Vo T, Gulati R. " Coughing chylothorax": traumatic non iatrogenic thoracic duct leak. Chest. 2022;162(4):A78. doi:10.1016/j.chest.2022.08.051
- Dar PM, Gamanagatti S, Priyadarshini P, Kumar S. Traumatic chylothorax: a dilemma to surgeons and interventionists. BMJ Case Reports CP. 2021;14(5):e238961. doi:10.1136/bcr-2020-238961
- Jindal R, Singh J, Garg L, Gupta M. Diagnosis and management of traumatic bilateral chylothorax: a clinical conundrum. BMJ Case Reports CP. 2019;12(7): e229400. doi:10.1136/bcr-2019-229400
- Hara H, Mihara M, Yamamoto M. Therapeutic lymphangiography for traumatic chylothorax. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2018 ;6(2):237-40. doi:10.1016/j.jvsv.2017.08.020
- Jahn HK, Frost JH, Van AS. Traumatic chylothorax in a young child: Case report and management. African Journal of Emergency Medicine. 2017;7(2):84-6. doi:10.1016/j.jvsv.2017.08.020
- Ghodrati A, Hassanzadeh M, Hassanzadeh M, Najafi Z, Akbarian HR. Traumatic Chylothorax: A case report. Journal of Torbat Heydariyeh University of Medical Sciences. 2016;4(3):55-8.
- Lee DH, Cho JY, Oh TH. Video-Assisted Thoracoscopic Ligation of the Thoracic Duct in a Patient with Traumatic Chylothorax. Journal of Trauma and Injury. 2016;29(3):89-92. doi:10.20408/jti.2016.29.3.89
- Sendama W, Shipley M. Traumatic chylothorax: A case report and review. Respiratory medicine case reports. 2015; 14:47-8. doi:10.1016/j.rmcr.2015.01.001
- Snow BD, Salcedo ES, Galante JM, Greenholz SK. Traumatic tension chylothorax in a child: A case report. Journal of Pediatric Surgery Case Reports. 2015;3(4):163-5. doi:10.1016/J.EPSC.2015.02.010
- Adams SR, Smith MI, Lee RM. Dyspnea and Pleural Effusion after a Motor Vehicle Accident: A Case of Traumatic Chylothorax. Proceedings of UCLA Healthcare. 2013;17 (1).
- Kumar S, Mishra B, Krishna A, Gupta A, Sagar S, Singhal M, et al. Nonoperative management of traumatic chylothorax. Indian Journal of Surgery. 2013; 75:465-8. doi:10.1007/s12262-012-0798-8
- Sharkey AJ, Rao JN. The successful use of octreotide in the treatment of traumatic chylothorax. Texas Heart Institute Journal. 2012;39(3):428.
- Kurklinsky AK, McEachen JC, Friese JL. Bilateral traumatic chylothorax treated by thoracic duct embolization: a rare treatment for an uncommon problem. Vascular Medicine. 2011;16(4):284-7. doi:10.1177/1358863x11408747
- Pandey R, Lee DF. Laparoscopic ligation of the thoracic duct for the treatment of traumatic chylothorax. Journal of Laparoendoscopic & Advanced Surgical Techniques. 2008;18(4):614-5. doi:10.1089/lap.2007.0243
- Robbins DH, Block M, Lewin D, Wallace M, Hoffman B. Control of traumatic chylothorax with EUS-guided thoracic duct injection sclerotherapy. Gastrointestinal Endoscopy. 2004 ;59(5): P212. doi:10.1016/S0016-5107(04)00971-X
- Buchan KG, Hosseinpour AR, Ritchie AJ. Thoracoscopic thoracic duct ligation for traumatic chylothorax. The Annals of Thoracic Surgery. 2001;72(4):1366-7. doi:10.1016/s0003-4975(00)02709-0
- Glyn-Jones S, Flynn J. Traumatic tension chylothorax. Injury. 2000;31(7):549-50. doi:10.1016/s0020-1383(00)00035-8
- Guleserian KJ, Gilchrist BF, Luks FI, Wesselhoeft CW, DeLuca FG. Child abuse as a cause of traumatic chylothorax. Journal of pediatric surgery. 1996;31(12):1696-7. doi:10.1016/s0022-3468(96)90054-8
- Fogli L, Gorini P, Belcastro S. Conservative management of traumatic chylothorax: a case report. Intensive care medicine. 1993; 19:176-7. doi:10.1007/bf01720537
- Grant P, Brown S. Traumatic chylothorax: a case report. Australian and New Zealand Journal of Surgery. 1991;61(10):798-800. doi:10.1111/j.1445-2197.1991.tb00155.x
- Brook MP, Dupree DW. Bilateral traumatic chylothorax. Annals of Emergency Medicine. 1988;17(1):69-72. doi:10.1016/s0196-0644(88)80508-0
- Krishnan MS, Jeyaratnam K. Traumatic chylothorax following a closed chest injury. Med. J. Malaysia. 1982;37(3): 270-72.
- Azambuja PC, Fragomeni LS. Traumatic chylothorax associated with subarachnoid-pleural fistula. Thorax. 1981;36(9):699.
- Rea D. Traumatic chylothorax in a closed chest injury: Report of a case. British Journal of Diseases of the Chest. 1960;54(1):82-5. doi:10.1016/S0007-0971(60)80048-4
- Guest DB. Traumatic chylothorax. Canadian Medical Association Journal. 1955 ;73(6):476.
- Elliot AW. Traumatic chylothorax. Canadian Medical Association Journal. 1954 ;70(1):71.
- Dorsey JF, Morris GE. Traumatic Rupture of The Thoracic Duct with Chylothorax: A Brief Review of The Literature. Journal of the American Medical Association. 1942;119(4):337-8. doi:10.1001/jama.1942.72830210001009
- Cellan-Jones CJ, Murphy W. Traumatic chylothorax. British Medical Journal. 1940 ;2(4165):590. doi:10.1136/bmj.2.4165.590
- Brown AL. Traumatic rupture of the thoracic duct with bilateral chylothorax and chylous ascites: New operation; report of a case. Archives of Surgery. 1937;34(1):120-8. doi:10.1001/archsurg.1937.01190070123006
- Bauersfeld EH. Traumatic chylothorax from ruptured thoracic duct: treated by intravenous injection of the aspirated chyle. Journal of the American Medical Association. 1937;109(1):16-8. doi:10.1001/jama.1937.02780270018005
- Lillie OR, Fox GW. Traumatic intrathoracic rupture of the thoracic duct with chylothorax: report of a case with recovery. Annals of Surgery. 1935;101(6):1367. doi:10.1097/00000658-193506000-00006
- Macnab DS, Scarlett EP. Traumatic chylothorax due to intrathoracic rupture of the thoracic duct. Canadian Medical Association Journal. 1932;27(1):29.
- Nakamura Y, Doi K, Fujii R, Ogura H, Umeda E, Kato T, et al. Postoperative constrictive pericarditis caused rupture of lymphatic collaterals: a rare etiology of chylothorax. General Thoracic and Cardiovascular Surgery Cases. 2023;2(1):81. doi:10.1186/s44215-023-00092-9
- Elsaied Hussein MH, Fadl Mahmoud I, Ms Eita Y, Ahmed Aglan MA, Esmaiel MSA, Abdelshafy Ibrahim Farag G, et al. A Prospective Study of Chest Trauma Scoring System as A Morbidity and Mortality Predictor in Patients with Blunt Chest Trauma. Med J Islam Repub Iran. 2024; 38:4. doi:10.47176/mjiri.38.4
- Baseer A, Noor N, Aman N, Qureshi AN. Utilizing Un-enhanced Chest Computed Tomography Screening for Blunt Trauma Surgery Decisions. Cureus. 2024;16(9):e69590. doi:10.7759/cureus.69590
- Elgar G, Smiley A, Latifi R. Major Risk Factors for Mortality in Elderly and Non-Elderly Adult Patients Emergently Admitted for Blunt Chest Wall Trauma: Hospital Length of Stay as an Independent Predictor. Int J Environ Res Public Health. 2022;19(14):8729. doi:10.3390/ijerph19148729
- Kakamad FH, Salih RQM, Mohammed SH, HamaSaeed AG, Mohammed DA, Jwamer VI, et al. Chylothorax caused by blunt chest trauma: a review of literature. Indian J Thorac Cardiovasc Surg. 2020;36(6):619-624. doi:10.1007/s12055-019-00904-0
- Nikbakhsh N, Zamani M, Noorbaran A, Naghshineh A, Rastergar-Nejad D. Etiological approach of chylothorax in Babol, northern Iran. Caspian J Intern Med. 2017;8(1):30-34.
- Air ME, Friedly J. Chylothorax complicating inpatient rehabilitation after thoracic spinal cord injury: a review of risk factors and anatomy for the physiatrist. Am J Phys Med Rehabil. 2012;91(12):1086-90. doi:10.1097/phm.0b013e31825f14c2
- Maldonado F, Cartin-Ceba R, Hawkins FJ, Ryu JH. Medical and surgical management of chylothorax and associated outcomes. The American journal of the medical sciences. 2010;339(4):314-8. doi:10.1097/maj.0b013e3181cdcd6c
- De Boo DW, Mott N, Lyon SM. Interventional Radiologic Management for Chylothorax. Clinical Pulmonary Medicine. 2015;22(1):25-30. doi:10.1097/CPM.0000000000000077
- Ebrahimian R, Souri Z, Feizkhah A, Mobayen M, Eslami Kenarsari H, Esmailzadeh M, et al. Evaluation of the Spiral Chest CT Scan Findings in Patients with Multiple Trauma. Bull Emerg Trauma. 2023;11(1):19-25.doi:10.30476/beat.2023.97214.1402
- Akgul Ozmen C, Onat S, Aycicek D. Radiologic findings of thoracic trauma. Therapeutics and clinical risk management. 2017:13:1085-9. doi:10.2147/TCRM.S143845
- Syed F, Khurshid Q, Wireko F, Poddar V. A Unique Case of Chylothorax Occurring Post-Chest Tube Insertion. Cureus. 2023;15(7):e41999. doi:10.7759/cureus.41999
- Bačić I, Morović D, Kovačić I, Vukosav D, Čulina Ž, Mihanović J. The contemporary approach to chylothorax–Single-center experience with the proposal of a management algorithm. Medica Jadertina. 2024;54(3):175-82. doi:10.57140/mj.54.3.4
Copyright (c) 2025 The Author(s)

This work is licensed under a Creative Commons Attribution 4.0 International License.


